There is often confusion with the terms Microbiota vs Microbiome. My aim is to clarify this for you so you have a better understanding of the unique environment which resides in all of us.
The Human Microbiota

This is often used to describe a particular colony of these organisms eg skin microbiome or gut microbiome and can also be used to describe the genes which are present in the microorganisms
Either way the terms are often interchanged and more often than not are used to describe the microorganisms present in the gut.
The Human Microbiome
This is often used to describe a particular colony of these organisms eg skin microbiome or gut microbiome and can also be used to describe the genes which are present in the microorganisms
Either way the terms are often interchanged and more often than not are used to describe the microorganisms present in the gut.
The Gut Microbiome
The human body could be thought of as a super organism as it is estimated the gut microbiome contains around 100 trillion microorganisms so there are many more foreign cells and genes in your body than your own. This synergistic relationship is crucial for human life and health.
There are some species of organisms which are more dominant than others but essentially all organisms live together for the greater good of your health and their survival.
Healthy Gut Bacteria
The term good bacteria and bad bacteria are often used to describe the gut environment, but essentially all bacteria are good and have an important role to play. It’s about balance and problems can occur if more pathogenic species start to proliferate and outnumber the beneficial species.
A surprising array of illness have been linked to an imbalance of diversity and ratios of good to less beneficial species of bacteria
These include
Bowel cancers, Immune based inflammatory bowel disease, auto immune diseases, cardiovascular disease, depression and even obesity.
There is a lot of exciting research happening in this area and in particular how the prevalence of specific species has been shown to increase specific disease risk.
Examples of Gut Bacteria
Akkermansia
Is a significant species of bacteria in our digestive tract. Akkermansia plays an important role in gut health by promoting and supporting mucosal health and mucous production.
It also is involved in creating healthy fuel for other gut microbes to feed on which in turn supports a healthy diverse microbiome.
As with all microorganisms in the gut, it is all about balance
Low levels of Akkermansia Muciniphilia have been associated with metabolic syndrome and obesity.
High levels have been associated with the autoimmune condition Multiple Sclerosis.

Helicobacter Pylori
This is a common bacterium present in approximately half of the world’s population.
When this bacterium is able to proliferate it can cause a huge range of gut symptoms including.
- Indigestion
- Pain
- Reflux
- Bloating
- Gastritis
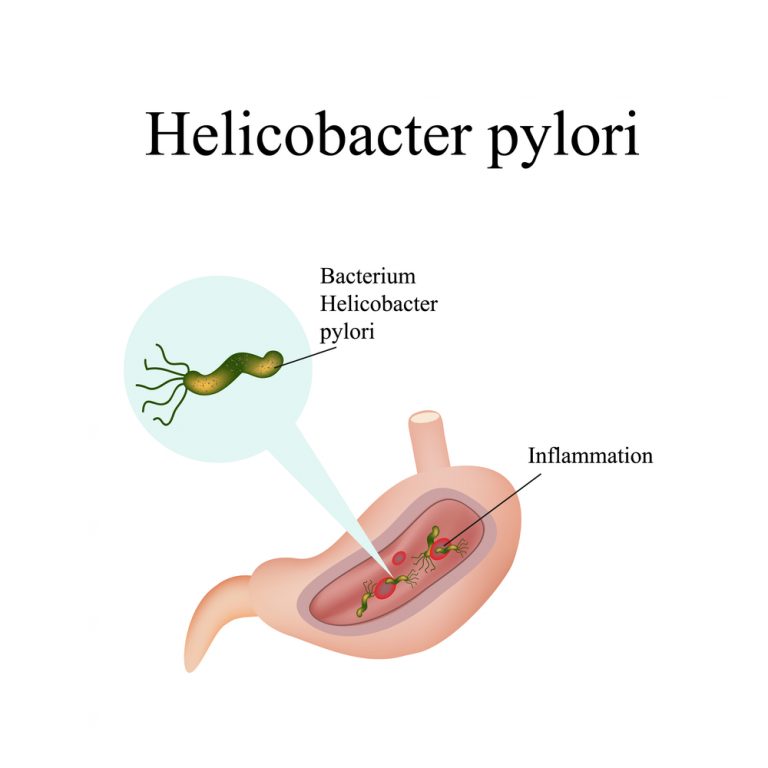
In 2005 Robin Warren and Barry Marshall were awarded a Nobel prize for their work on H pylori and its causal link to gastric ulcers and gastric cancer.
Their work has meant the treatment protocol for gastric ulcers has changed with a focus on reducing or eliminating H pylori with antibiotics.
Not everyone with H pylori gets symptoms and not everyone with h pylori gets ulcers or gastric cancer.
There are many contributing factors including overall health, stress and acid levels in the gut.
Yersinia Enterocolotica
Yersinia is a bacterium in the family of bacteria called Enterobacteriaceae. This family of bacteria are known to cause infections in animals as well as humans. Exposure to this bacterium can come from undercooked meat and contaminated water.
Infection with Yersinia has been associated with auto immune Thyroid diseases including Hashimoto’,s Thyroiditis and Grave’s disease . High antibodies to Yersinia have been found in patients with these disorders and who also have a genetic predisposition to the condition.
Yersinia Enterocolotica has also been associated with some cases of reactive arthritis.
Yesinia can also mimic other health conditions such as inflammatory bowel disease.

Clostridium difficile
Clostridium difficile also known as C. diff is a well-known pathogenic bacterium that can cause diarrhoea and pain in the Gi tract. It can sometimes take hold after antibiotic use when there has been considerable disturbance to the microbiome.
C diff can cause sever inflammation in the gut and can cause colitis
It is an infection that is commonly caught in hospital
Klebsiella
Klebsiella is considered to be a bacteria normally found in a healthy GI tract. However like so many other species in the microbiota, it is about the number and balance of flora
High levels have been associated with increase histamine and gut inflammation. It is also a species implicated as an auto immune trigger in conditions such as Rheumatoid arthritis and Ankylosing Spondylitis.